What is the Diabetes Honeymoon Phase
The diabetes honeymoon phase, also known as the remission phase, is a period that can occur shortly after the diagnosis of type 1 diabetes, and sometimes type 2 diabetes. During this time, the body still produces some insulin, leading to a temporary decrease in the amount of insulin needed to manage blood sugar levels. Understanding this phase is crucial for effective diabetes management and setting realistic expectations.
Defining the Honeymoon Phase
The honeymoon phase is characterized by a period of improved blood sugar control with a reduced need for exogenous insulin. This happens because the body’s remaining insulin-producing cells (beta cells in the pancreas) are still functioning to some extent. This phase can vary in length, and not everyone experiences it. It’s a time when the newly diagnosed individual might feel a sense of relief, as they require less insulin and experience fewer fluctuations in blood sugar.
Duration of the Honeymoon Phase

The duration of the honeymoon phase is highly variable. It can last for a few weeks, several months, or even a year or more. The length of the phase depends on factors such as the individual’s age, the severity of the initial diagnosis, and the effectiveness of the initial diabetes management plan. Ultimately, the honeymoon phase is temporary, and the body will eventually require more insulin to manage blood glucose levels as the beta cells gradually decline.
5 Surprising Facts About the Diabetes Honeymoon Phase
Fact 1 Reduced Insulin Needs
One of the most notable aspects of the honeymoon phase is the significantly reduced insulin requirements. Individuals often find that their insulin dosages decrease, and they may experience fewer instances of high or low blood sugar. This is a welcome change and can provide a sense of normalcy as the body is still producing some of its own insulin. Careful monitoring is essential during this time to avoid over-medication and potential complications.
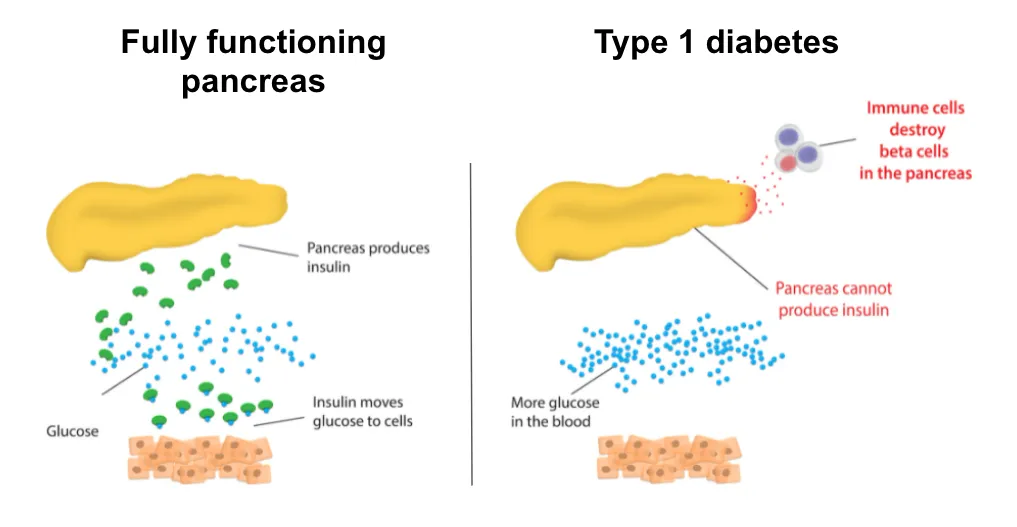
Understanding Insulin Production

Insulin is a hormone produced by the beta cells in the pancreas, and it is essential for regulating blood sugar levels. In type 1 diabetes, the immune system attacks and destroys these beta cells, leading to a lack of insulin production. During the honeymoon phase, a small number of these beta cells may still be functioning or recovering, leading to some insulin production.
The Role of Beta Cells
Beta cells are the key to insulin production. During the honeymoon phase, these cells are still alive and able to function to some degree, which explains the reduced insulin needs. Preserving these beta cells, if possible, is an important goal of treatment during this initial phase, but eventually, the body’s ability to produce insulin will continue to decline, and a return to a more stable insulin regimen will be necessary.
Fact 2 Fluctuating Blood Sugar Levels
Despite the reduced insulin needs, blood sugar levels during the honeymoon phase can still be unpredictable and fluctuate. This is because the remaining beta cells may not consistently produce insulin, leading to periods of high and low blood sugar. The individual may experience blood sugar swings, especially after meals or during exercise. Careful monitoring, dietary adjustments, and proactive insulin adjustments, under the guidance of a healthcare professional, are essential.
Impact of Diet and Exercise
Diet and exercise play a critical role in managing blood sugar during the honeymoon phase. Dietary changes, such as a reduced intake of carbohydrates and sugars, can help to stabilize blood sugar levels. Regular physical activity can also improve insulin sensitivity, potentially reducing the need for insulin. It’s important to work with a healthcare team to develop a personalized plan.
Managing Blood Sugar Swings
To manage blood sugar swings, regular blood glucose monitoring is essential. Adjusting insulin dosages, based on blood sugar readings and carb intake, can also help to stabilize levels. It’s important to learn to recognize the patterns of blood sugar fluctuations, such as the impact of certain foods or activities. A healthcare team can provide guidance on these adjustments.
Fact 3 Risk of Hypoglycemia
Hypoglycemia (low blood sugar) is a significant risk during the honeymoon phase due to the reduced insulin needs and potential for over-medication. As the body is still producing some insulin, it’s essential to be vigilant about the signs and symptoms of low blood sugar, and to respond quickly if it occurs. Over-treatment with insulin or missing meals are common causes, and it’s important to avoid these pitfalls.
Recognizing Hypoglycemia Symptoms

Symptoms of hypoglycemia include shakiness, sweating, dizziness, confusion, and hunger. Recognizing these symptoms and acting promptly is crucial. If you suspect hypoglycemia, check your blood sugar immediately. If it’s low, treat it with fast-acting carbohydrates, such as glucose tablets or juice. Carry a source of fast-acting glucose at all times.
Treating Low Blood Sugar
Treating low blood sugar involves consuming 15-20 grams of fast-acting carbohydrates, then waiting 15 minutes and rechecking the blood sugar. If the blood sugar is still low, repeat the process. Once blood sugar is within the target range, have a snack to stabilize levels. Severe hypoglycemia requires immediate medical attention, and can lead to loss of consciousness, seizures, and, in rare cases, death.
Fact 4 The Importance of Continued Monitoring
Even during the honeymoon phase, regular blood glucose monitoring is non-negotiable. Monitoring helps individuals understand their blood sugar patterns, adjust insulin dosages as needed, and prevent complications. It’s crucial to work with your healthcare team to establish a monitoring schedule and interpret the results. Maintaining this practice is important even when the need for insulin decreases, and the individual feels better.
Regular Blood Glucose Checks

Regular blood glucose checks should be performed throughout the day, including before meals, before bed, and sometimes after meals and during exercise, as recommended by your healthcare provider. The frequency of checks may vary depending on your individual needs. Accurate blood sugar monitoring is crucial for adjusting insulin dosages and preventing complications.
A1C Testing
A1C testing provides an average of blood sugar levels over the past two to three months. This test is an important tool for assessing overall blood sugar control. The frequency of A1C testing typically is every three months, but it should be performed at the discretion of the healthcare team. It’s important to maintain a healthy A1C level to reduce the risk of long-term diabetes complications.
Fact 5 Lifestyle Adjustments
During the honeymoon phase, lifestyle adjustments are crucial to manage blood sugar levels. This includes dietary changes, regular exercise, and stress management. While the individual may need less insulin during this phase, these lifestyle factors continue to significantly impact blood sugar control. The goal of this stage is to make the lifestyle adjustments as easy as possible.
Dietary Changes
Dietary changes should focus on balanced meals, including portion control, carbohydrate counting, and choosing foods with a low glycemic index. Reducing intake of processed foods, sugary drinks, and refined carbohydrates can help stabilize blood sugar levels. Work with a registered dietitian to create a personalized meal plan that meets your individual needs and preferences.
Exercise and Diabetes
Regular exercise improves insulin sensitivity, helping to lower blood sugar levels. Aim for at least 150 minutes of moderate-intensity exercise per week, such as brisk walking, cycling, or swimming. Monitor blood sugar levels before, during, and after exercise to understand how your body responds. Adjust insulin or carbohydrate intake accordingly. Consult with your healthcare team to design a safe and effective exercise plan.
Tips for Managing the Honeymoon Phase
Managing the honeymoon phase effectively requires careful planning, regular monitoring, and open communication with your healthcare team. By staying informed and proactive, individuals can make the most of this phase and reduce the chances of complications. This phase is a unique experience and one that individuals should prepare for in order to be successful.
Working with Your Healthcare Team
Regular check-ups with your endocrinologist, diabetes educator, and other members of your healthcare team are essential. They can help you monitor your blood sugar levels, adjust your treatment plan as needed, and provide support and guidance. Communicate any concerns or questions you may have. The honeymoon phase can create many questions that require answers.
Education and Support
Seek out education and support from diabetes educators, support groups, and online communities. Learning about diabetes and sharing experiences with others can provide valuable insights and help you feel less alone. The healthcare team can often point individuals in the right direction. Knowledge is power when living with diabetes.
Long-Term Outlook for People with Diabetes
The honeymoon phase is temporary, but it doesn’t define the long-term outlook for people with diabetes. Effective diabetes management, including insulin therapy, lifestyle adjustments, and regular monitoring, is critical to maintaining good health. With proactive management and support from a healthcare team, individuals with diabetes can lead long, healthy, and fulfilling lives. Remember the importance of patient support groups as well. The honeymoon phase may end, but the journey continues.